Introduction
The American Society of Hematology (ASH) guidelines recommend rapid (within 1 hour) administration of tailored pain medication and frequent reassessments to optimize pain control in persons with sickle cell disease (SCD) presenting with acute pain related to SCD (Brandow et al., 2020). Implementation of an individualized pain plan (IPP) has been associated with decreased length of stay and lower rate of 7-day readmissions (Welch-Coltrane et al., 2021).Early initiation of sustained analgesia results in more rapid resolution of vaso-occlusive crises (VOC) in 80% patients. While all of our patients have an IPP, provider knowledge of the existence of IPPs and where to find them has been challenging to properly implement this practice. All inpatient SCD patients receive hematology consults but lack of continuity and experience with patients can be challenging for them.
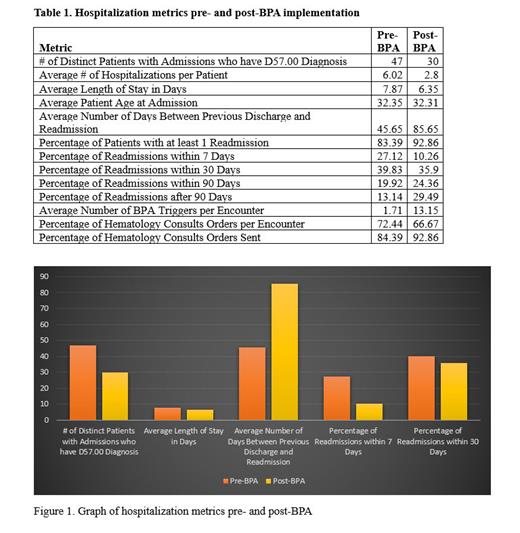
The study aimed to investigate the impact of implementing a Best Practice Alert (BPA) and introduction of dedicated SCD nurse practitioner (NP) on consults on various clinical metrics related to patients with sickle cell disease during hospitalization.
Methods
We created a best practice alert (BPA) that is triggered when a patient with SCD is admitted to the inpatient service. It directs the admitting team and nursing staff to the IPP and an order set for sickle cell pain crisis. The nursing interface of the BPA also includes a link to an educational module. Data was collected pertaining to length of stay, readmission, and percentage of admissions with a hematology consult placed from before and after implementation of the BPA. Around the same time, a dedicated nurse practitioner managed consults for patients hospitalized with sickle cell VOC and provided education to the primary team. We then conducted a retrospective chart review of all sickle cell patients at the University of Wisconsin from January 1, 2021, to December 31, 2023. We included all patients 18 years and greater with a sickle cell disease diagnosis as identified by the ICD-10 code (D57.00) and excluded patients with restricted research participation. We used descriptive statistics to obtain summaries of patient demographics as percentages for categorical variables and mean values for continuous data.
Results
Preliminary data demonstrated that the number of distinct patients with admissions decreased from 47 pre-BPA to 30 post-BPA (Table 1, Figure 1). The average length of stay in days decreased with 7.87 days pre-BPA to 6.35 days post-BPA. The average number of days between previous discharge and readmission increased from 45.65 to 85.65 after implementation. Readmissions at 7 and 30 days decreased by 17% and 4%, respectively.
Conclusion
The goal of this QI initiative was to improve IPP implementation by introducing a BPA in the chart directing admitting providers to the plan for efficient use. Dedicated SCD NP provided continuity and ensured IPPs were followed. While we could not directly measure the implementation of IPP with each BPA trigger, relevant patient-related outcomes such as readmissions and length of stay were reduced with meaningful reduction in LOS by 1.52 days during the first 9 months of these changes. In the future, we plan to further refine this process and expand our outcomes data by obtaining patient and provider feedback via surveys to fully understand the impact of this process and continue improvements. The role of SCD NP will be expanded due to encouraging results. In summary, BPA alerts in the chart for rapid implementation of IPPs, along with a knowledgeable SCD consult provider to ensure proper follow up of plans is a feasible strategy to improve patient outcomes when admitted with VOC.
Disclosures
No relevant conflicts of interest to declare.